This blog-post was started in late November or early December 2021. It takes me a long time to single-finger type. Any kind of active and deep-thinking uses energy, and we people with Myalgic Encephalomyelitis (pwME) have a chronic lack of energy, especially so for me and many other pwME during the Winter months. I have over one hundred distinct conditions/symptoms, most of which are subsumed into the M.E. rubric.
HEALTH BACKGROUND
I was retired on ill-health grounds in the late 1990s after developing disabling conditions. These mostly have been on a deteriorating trajectory over the past two or so decades. I wrote a blog-post detailing my conditions and major symptoms entitled, International M.E. Awareness Day 2020 . A copy of the original (uncensored) document is held by Trafford Council’s social-services department and additionally a copy was sent to the Trafford-owned care-agency.
In December 2020 I wrote to the Director of Trafford Social Services:
“I have Myalgic Encephalomyelitis (ME). Initially diagnosed by my then G.P., Dr. {name of G.P.} at {name of medical-centre} (currently also Medical Director at {name} CCG). Confirmed by ENDOCRINOLOGY dept. at {name of hospital A}. I have the severe form as listed in the current NICE guideline.
I have Fibromyalgia (FMS). Diagnosed by RHEUMATOLOGY dept. at {name of hospital B}.
I have Hypermobility & Osteoarthritis (OA) of my left hip. Diagnosed by RHEUMATOLOGY dept. at {name of hospital C}.
I have OA of my lower spine. Diagnosed by RHEUMATOLOGY dept. at {name of hospital B}.
I have several other Arthritides. Diagnosed by my current G.P., Dr. {name} at {name of medical-centre}.
I have several other conditions and dozens of symptoms/co-morbidities. These are detailed in a spreadsheet, supplied to Social Services.
I received a support package from the late Trafford PCT. Apparently it was only the second time such a package was approved by the PCT prior to its demise.
The Department for Work & Pensions (DWP) considers I am so chronically sick/disabled that they granted me a ten-year bye from annual reviews for social-security benefits.
To sum: I am considered by NHS consultants, G.P.s and other official bodies to be severely disabled & chronically sick.”
DIFFICULTIES OBTAINING APPROPRIATE CARE-SUPPORT
Obtaining appropriate care-support from my local authority has been a constant battle. Social-services do not appear to learn from errors made nor do they appear to have full access to files/correspondence. This means a constant repeating of information/enquiries/investigations/etc.
In February 2017 I wrote a couple of blogposts entitled, Disability Discrimination in Trafford and No Food, no Meds, no Care in Trafford .
In April 2017 I wrote a further blog, Disablies are Dying in the UK .
One example of these issues is the repeated sending round of male carers despite explicit instructions not to do so, due to my sexual assault & rape issues. They investigate, apologise, promise it will not re-occur, and then it happens again and again. Each time igniting PTSD for several days or even weeks.
COGNITIVE ISSUES
I have various conditions/symptoms that militate against clear-thinking. In my FAQ document provided to both Trafford social-services and the Trafford Council-owned care-agency, I provided the following information.
Under “Memory”:
“Colin generally has no issue with long-term memory, except when tired. However, his short-term memory can be exceptionally poor. For this reason, carers need to prompt with precise questions rather than generalised and open questioning. For example, “Do you need anything?” will never elicit a positive response. Ask, “Do you need to clean your teeth.” See also Dyscognition.”
Under “Dyscognition”:
“There are times when Colin is brain-fogged, which can cause dyslexia, dyspraxia and a loss of vocabulary for everyday items and names of even folk he knows well. This is a symptom of his conditions. Worry not!”
In short, I have severe issues with ‘active-memory’: if I am given meds to take, I meed to be watched to ensure I take them and do not simply put them down. I do know that I need to take them, but in the moment I completely forget. It is well known that many if not most pwME suffer to varying degrees with this aspect of recall. I have severe M.E. and thus might be expected to have more severe problems in recalling actions etc. This issue of poor active-memory is the main reason why prompting devices are inappropriate - for they cannot ensure an action is taken!
Typically, although not invariably, over the past two decades plus, I have become more cognitively aware approximately 18.00-19.00 to 21.00-22.00 depending on season, weather, etc. During this period I concentrate on eating my main meal of the day. I have difficulties in co-ordinating cutlery/vessels to my mouth, so dining of itself becomes a taxing activity. Generally after waking, whether after the night or a nap, I am very groggy for quite some time. Thus, a carer waking me at 16.00 (or previously at 11.00) is not going to obtain much sense from me until I have my bearings. This latter can take a couple of hours or so.
Trafford social-services have been made aware repeatedly. However, they insist on turning up when I am very unlikely to be in a position to know what they want and unable to remember much if anything of such encounters. The social-workers invariably think they know best and ignore this. In 2020, social-workers turned up in the morning and I lodged a formal complaint (the partial letter above is from same). Obviously it was ignored, as a few weeks back, yet again, they turned up earlier in the day. I repeatedly had to ask them to leave, but they insisted on continuing to put question after question.
MENTAL HEALTH
Background
I have a personal history of mental-health issues including OCD, Anxiety, Social-Anxiety, Depression and multiple suicide-attempts. I have a personal history of child-abuse, teenage-abuse, adult-abuse, sexual-assaults and rapes. At the end of the 1990s, after my last suicide-attempt and a mental-breakdown, I was hospitalised to give me a space in which to recover. From this I was referred to a local Mental-Health Trust. A wonderfully supportive psychologist spent a year using CBT-techniques to help bring me back into the outside world.
Depression
Since 2000, I have only once been sufficiently depressed to request (prescription-medicine only) support from my G.P. This occurred after moving home, the second-most stressful type of event after separation/divorce. It lasted but a few months whilst I became comfortable in my new world. As soon as I felt able, I apprised my G.P. that I was reducing the depression meds in order to fully come off them.
Anxiety
On the other hand, I have periodic prolonged anxiety, at which points I have contacted my G.P. to increase my anti-anxiety medication. Similarly, once I have felt more my normal self, I have then requested a reduction in the medication.
However, when I last wrote to the selfsame G.P., she advised me that we are all extra stressed at the moment and did nothing for me.
Suicidal Ideation
I have moved from being circa 85% bed-bound to some 95% bedridden. In Autumn of 2019, my G.P. agreed to refer me for a new inside wheelchair. My current chair is too large and unwieldy for use inside. I am still waiting for a referral. Had I had a usable wheelchair during these past couple of years, I could have gone downstairs more frequently, even out into my disabled-friendly garden constructed to support my needs. Instead I am trapped in what I cutely call my “bed-cell”!
I have increasingly been plagued by intrusive thoughts about suicide, dreams about my own or friends’ suicides and a waxing-waning obsession with death.
However, if my own G.P. is reluctant to support me, I really feel hopeless about my situation going forward.
CHANGE IN CARE-AGENCIES
Background
Covid hit my previous (good) care-agency hard. Best At Home Adult Care found it impossible to cover nights due to a loss of staff under the pandemic.
“A new stressor for me to add to my anxiety: my carer agency has to give up my contract along with several others. This is due to lack of staff. Most folk do not want to work nights. I should suggest giving a premium for working these shifts, but local councils do not have the money in the massively underfunded social-care system. I feel really upset about losing carers who have become such good friends. This has been the best agency I have yet experienced. Fingers crossed that the next one is just as good - or even better!” (07.08.00)
I went through four care-agencies in approximately eight months, from August 2020 to April 2021. For a person with social-anxiety & anxiety the never-ending revolving staff obviously caused a deterioration in my health, both mental & physical. I lodged several complaints with Trafford Council over the poor care from the carer-agencies, with issues which included carers not having sufficient proficiency in spoken English to be able to comprehend what was required of them and me having to revert to speaking French and even Italian (which I do not really speak) or to having to use Google images.
Failures
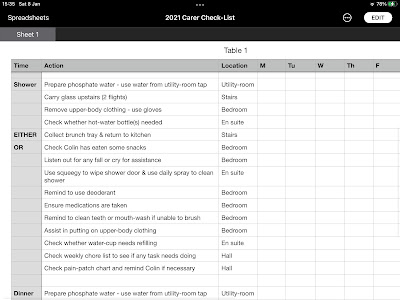
Despite each agency and Trafford social-services being provided with detailed lists of duties & requirements (a couple of examples of daily duties appear below), none of the last three care-agencies (including the Trafford Council-owned agency) have followed the lists. The result is that: I am rarely reminded to wash; I am almost never reminded to clean teeth/mouth; I am often not reminded and helped to change clothing; I am often not fed in the afternoon (my first call of the day) unless I remember to ask. And so on.
CHANGES TO MY CARE REGIMEN
From August 2020 (without any consultation with myself) to the current date, the council-owned care-agency, with Trafford social-services’ backing, cancelled my morning-call at 11.00. I now only have calls at 16.00 and 18.00. There have been multiple effects.
Eating
Since the late 1990s I have not experienced hunger. No hunger-pangs. No physiological prompt to eat. If a person does not prompt me to do so, I fail to consume food. To make matters worse, on waking I generally suffer from nausea for a couple of hours.
I mostly only eat one meal per day at 20.00 when my housemate cooks and brings up a hot-meal. When he is not here, carers take on the duty. I get a snack at 16.00 if I recall to request and sometimes carers prompt, but not consistently. Best At Home Adult Care Managed to have me eating two or three times every day. I regularly, although not daily due to the nausea, ate breakfast. Additionally, a bowl of mainly fruit snacks on the bed, meant I was constantly reminded to eat. Most days I would finish the bowl. Now a bowl lasts several days due to the changes in care-regimen, failure to prompt and failure to check what I have eaten. In other words I am at risk of malnutrition. Indeed, I recorded & reported a large drop in weight under the current regimen, but nought has been done to ameliorate the matter.
Additionally due to the change in medicating caused by cancelling the morning-call - when the medications ought to be correctly taken - I have to wait a minimum of thirty minutes prior to eating the snack. THIS RATHER OBVIOUSLY MEANS NO HOT-FOOD! However my cognitive issues and lack of any appetite for over two decades, mean I very often forget to eat the snack until around 18.00 - 19.00 when I begin to be more cognitively aware of my surroundings, etc. In other words, even when actually being given two meals, I eat them within one to two hours of each other.
Water
For months I was left consuming only four cups of water per day, two of which were medicated. This is massively below the NHS recommended daily fluid intake for adults. From 20.00 until the next call the following day at 16.00, i.e. some twenty hours I was left without hydration. Due to inter alia poor fine-motor skills, poor strength, poor co-ordination and so forth, I cannot use a jug, bottle or thermos. A charity heard of my plight and sent me a hydration-system.
However, I always thought I did get thirsty, but it now appears that mostly I do not, unless ill or extra hot. It seems it was the prompting by carers and the routine that had me drinking. The routine has now long-since been broken. The current carers note that I often hardly touch my water.
I contacted my G.P., as obviously extended lack of water is bound to cause ill-health effects. They advised that the matter is NOT medical and as such washed her hands of the issue. I enquired as to why after several months they had not provided hydration-powders or similar, and response came their none other than to go to A&E if I felt I needed to. As a bedridden person this was laughable advice and really rather condescending.
Medications
G.P. Review
My G.P. reviewed and altered my prescription in the Summer of 2021. They did not contact to advise me that they were undertaking a review. They did not contact me for my input. They did not contact me to advise me they had altered the prescription. They did not even undertake to carry out blood-investigations prior to making any changes. I only discovered that changes had occurred when carers began to use the revised protocol. To this day I have still had no explanation as to what occurred and the reasoning behind doing a review without blood-tests and the patient’s in-put.
Effects
Taking medication at teatime that ought to be taken in the morning has had several effects.
Increased nausea, heart-burn and acid-reflux due to the relevant medication being taken too late in the day.
Almost constant sleep-disturbances at night as evidenced my my Fitbit records pre- & post-changes to the medicating programme. I now wake up almost every wee-small-hours. This is a known side-effect of moving my anti-anxiety med to later in the day instead of in the morning.
A massive reduction in the sleep I obtain, almost half of what I normally obtain at this time of year, which cumulatively is having an adverse effect on my mental-health and stress-levels.
My G.P. has not taken any blood for testing in the months since the changes to check whether the changes have had any effect on my hypophosphatæmia & hypocalcæmia.
Pharmacist
It should be noted that, despite pressure form the council-owned care-agency &/or social-services, my pharmacist has refused to move the medications from the morning section of the blister-packs to the teatime section, for, as they assert, the meds need to be taken in the mornings.
Migraines
I have had classic migraines since being an older child, about eleven or twelve. I have now developed almost daily migraines including classic, stomach & retinal. I wrote to my G.P. for support, but there has been no alteration to my current six tablets every four weeks. In other words, mostly I have to put up with the migraines and the ensuing vomiting etc.
The latter must also be contributing to my on-going levels of hydration etc.
Itching & Rashes
I have had an exponential increase in rashes & itching, which are probably related to stress.
Medicated-Water
The reduction in my medicated water, from thrice per day to twice (but taken in a narrow time-frame), has resulted in an increase in muscle ticks, spasms, pins & needles and especially cramps. This med had all but controlled these symptoms whilst being administered three times daily spread throughout the day for the past decade or so.
I made my G.P. aware of the above, but they made no alteration to the prescription nor did they give me an explanation as to their reasoning.
Bedridden
I have gone from being bedridden some 85% of the time to about 95+% since the régime-change. I have not been downstairs in some seven to eight weeks. Previously I would make it downstairs every 10-14 days. I mostly stagger to my en suite (3m) or have to use a urine-bottle.
Relationship
My friendship with my housemate has been severely stressed. He has been thrust into a care-rôle he did not request nor has he elicited the responsibilities. Neither has Trafford social-services contacted him to discuss the matter - not once in something like a decade! Typically, I only see and speak to him for around five to ten minutes in the evening, when he brings up my evening-meal. The strain is palpable. He has become moody, argumentative and unpredictable. It is additionally yet another stressor to add to my anxieties.
Complaints
I have made complaints to the care-agency, social-services and Trafford Council. As there has been no alteration nor amelioration in my situation, I must assume that they were not taken seriously enough.
ANALGESIA
Background
For my worst pain, in my lower spine caused by inter alia OA, M.E. & Fibromyalgia, I am prescribed pain-patches. I also take (with G.P. consent) over-the-counter painkillers and other prescription analgesics for other pain caused by inter alia several arthritides.
Pain-Patches
Due to sensitive skin and resultant adverse reäctions, my G.P. agreed to a shorter change-cycle in May 2021. Since then they have made no enquiries as to how I am faring under this changed regimen.
Controlled-Drugs
For my worst pain I am prescribed a controlled-drug, which is a pain in itself to source, whether it be the prescription off the G.P. or the pharmacist having issues obtaining the specific medicine. I advised my G.P. back in 2021 that due to various changes in care I was suffering and continue to suffer increased pain-levels. My G.P., despite a request to do so, has not increased my prescription nor apprised me as to the reasons therefor.
Physiotherapy
I suffer many skeletal and muscular issues due to many of my conditions and their interaction. I especially suffer from Costochondritis and this really impacts my ability to breathe comfortably and pain-free. Due to being being almost totally bedridden now, I have been unable to visit my private physiotherapist for over two years. The council-owned agency advised that G.P.s can arrange therapy at home. Despite writing to my G.P. about this matter, they have not arranged any support and thus relief.
Non-Medicinal Pain-Relief
For some two decades I have used a lightly-filled hot water-bottle (HWB) under my spine. I have almost no curvature of the spine (rather like our C19th ancestors) and as such the care-agency’s suggestion of a heated bean-bag is exceedingly uncomfortable to downright painful in itself, for I have almost no flesh in the area, after some two decades of lying flat.
I also used HWBs to alleviate the symptoms of IBS. Whilst it is true that heated bean-bags do give initial relief, this only lasts around thirty minutes, whereas a HWB lasts a couple of hours. The refusal to give HWBs means I am forced to take more medicines in an effort to reduce pain.
In 2021 I asked for advice from my G.P., but none has there come.
It is worth pointing out here, that in almost twenty-five years of being bedridden, neither my current G.P. (15+ years), nor my previous G.P. (10+ years), nor any of the NHS hospital consultants in the three/four hospitals I have attended have ever provided any advice on dealing with being bed-bound. For example, I now lie on a sheepskin in order to reduce sensitivity and pain - I learned this tip from other chronically-ill folk. I have never had any diëtary advice on foods to consume or avoid in order to reduce auto-immune inflammation. And so forth…
ACTIONS TAKEN
At this time of year, for the most part: I cannot watch television due to vision issues; I cannot listen to the radio or music due to hearing issues; I cannot think for extended periods due to cognitive issues; I cannot type more than a few sentences & cannot hand-write at all due to physical issues; I cannot read extended test (i.e. more than a short paragraph) due to cognitive &/or vision issues.
Any stress makes me sleepy &/or fall asleep. I have to avoid angst whether in the news or in a drama. Almost anything at the moment can set off a panic-attack. I am doing my best to remain calm and avoid as many stressors as possible.
For months, when able, I have been tweeting the Care Quality Commission, which supposedly has oversight of care-agencies and council social-services departments. (See here.)
I have kept Trafford Council included in many of the tweets. The relevant council-person who oversees adult-care in Trafford refuses to be tagged. Apparently she is aware of all issues: yet there has been no amelioration in my situation?
There is little, if any, effective communication between my G.P., Trafford social-services & the Trafford-owned care-agency.
I made several outreaches to the Manchester Evening News (M.E.N.) - but no come-back from them about the national #SocialCareCrisis. Perhaps they are inundated with such tales?
FUTURE ACTIONS?
Who can I actually turn to for genuine help & support - not just words?
Were I to commit a crime: I should be fed three times per day; I should receive my meds three times per day; I should be kept hydrated; I should receive appropriate medical-support; I should receive hygiene support twice per day; I should have assistance changing my clothing daily; and so on… I should even be taken outside into the fresh-air in my outside wheelchair.
As a chronically-sick & disabled person I am all but ignored.
Logically I ought to commit sufficient crime to be incarcerated - any suggestions? The alternative, regrettably, is suicide as starving to death is very painful. Crime or death by my own hand or death via malnutrition/dehydration? Crime or death.
My outrider notion is to claim asylum in Scotland. Can an English-person do so? Crime or death or asylum!





No comments:
Post a Comment